MPS VII is a rare and progressive inherited disease1,2
MPS VII is a form of mucopolysaccharidosis (MPS), a lysosomal storage disorder. It may affect every single patient differently and impacts the organs, bones, and other parts of the body.1,2
What happens in MPS VII?
People with MPS VII do not make enough of a specific enzyme in their cells, called GUSB (β-glucuronidase). GUSB breaks down and recycles GAGs (glycosaminoglycans).2,3
GAGs are cellular waste that builds up in lysosomes in cells. GAGs collect in organs, bones, and other parts of the body. If they are not broken down, they can cause progressive multi-organ problems.2,3
Healthy cell
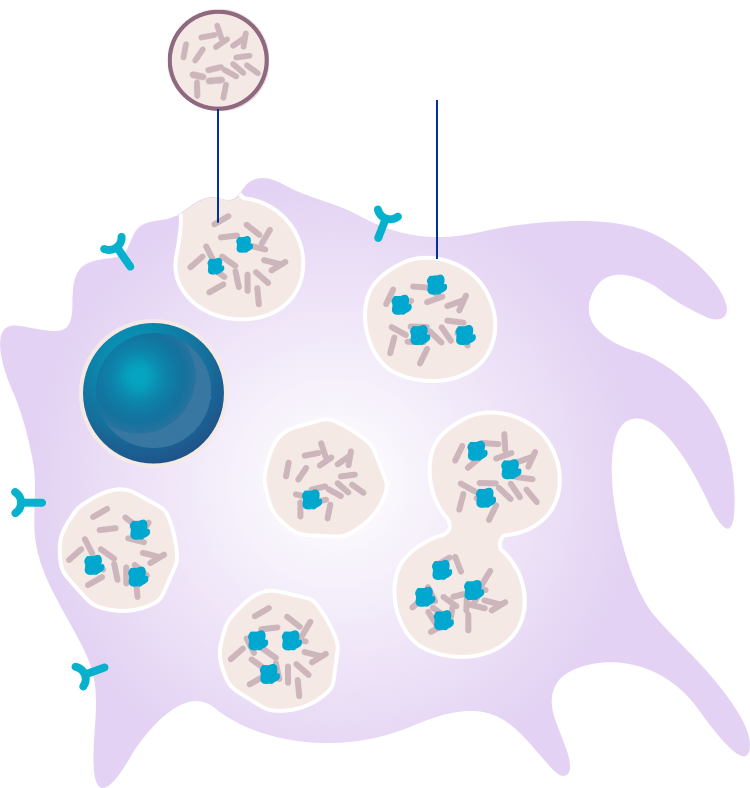
GAGs are contained within a certain part of the cell called lysosomes.
Diseased cell
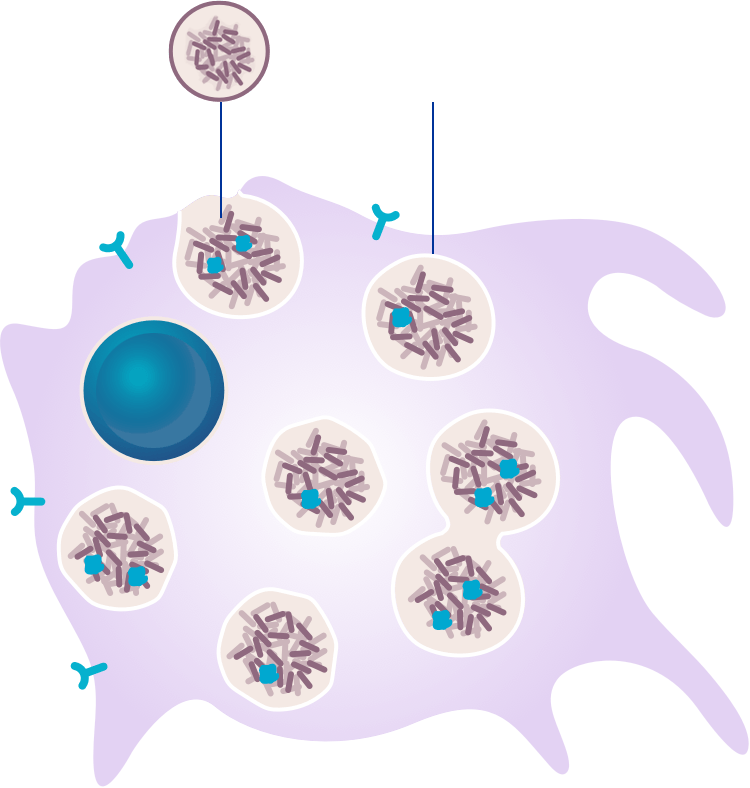
GAGs accumulate in cells throughout the body, affecting many systems, including bones, tissues, and organs.2-4
MPS VII is a rare genetic disease1,2
Fewer than 1 in 1,000,000 people have MPS VII.5
MPS VII is inherited in an autosomal recessive manner6
Inherited means the mutated gene that causes the enzyme deficiency, called the GUSB (β-glucuronidase) gene, is passed down from parent to child.1,6
Autosomal recessive describes the way the genes are passed down. In this case, two copies of the abnormal GUSB gene, one from each parent, must be present for a child to be born with MPS VII.1,6
If both parents are carriers of the mutated GUSB gene, there is a 1 in 4 chance each child will be born with MPS VII6
 |  | ||
| Genetic carrier | Genetic carrier | ||
 |  |  |  |
| Noncarrier, not affected | Genetic carriers, not affected | Affected | |
Signs and symptoms of MPS VII
The signs and symptoms of MPS VII vary from person to person2,4
There is a wide spectrum of MPS VII symptoms. For some people, symptoms begin early, and for others, they develop progressively later in life.1,2,6
Common signs and symptoms of MPS VII
MPS VII affects many of the body’s systems. Signs and symptoms may begin prenatally and during early childhood and include the following:2,6
1. Neurological symptoms1
Developmental delay and intellectual disabillity
2. Ear, nose, and throat signs2
Coarse facial features, increased head circumference, short neck, coarse hair, ear and respiratory infections, enlarged tongue, and hearing loss
3. Gastrointestinal signs2
Enlarged liver and spleen, hernias, diarrhea, difficulty in swallowing, heartburn, and intestinal inflammation
4. Musculoskeletal issues2,7
Abnormal development of all bones, joint pain and stiffness, short stature, joint contracture, scoliosis, kyphosis, hump, knock-knee, curved fingers, and restricted mobility
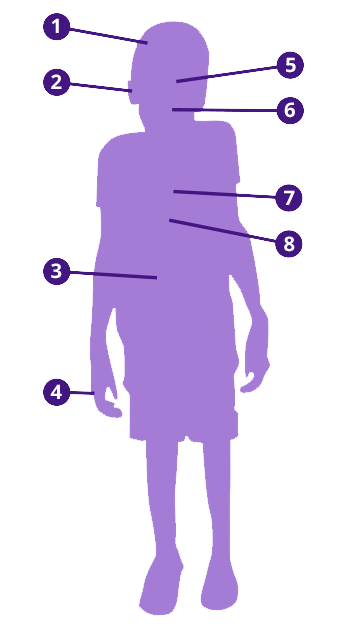
5. Ophthalmological complications2
Corneal clouding, heavy eyebrows, visual impairment, and photosensitivity
6. Dental issues2
Abnormal dentition with small and widely spaced teeth and enlarged gingiva
7. Cardiovascular signs2
Left ventricular hypertrophy, aortic insufficiency, mitral regurgitation, congestive cardiac failure, aortic stenosis, and thickened aortic and mitral valves
8. Pulmonary complications2,7
Decreased pulmonary function, obstructive airway disease, sleep apnea, and chronic bronchitis
1. Neurological symptoms1
Developmental delay and intellectual disabillity
2. Ear, nose, and throat signs2
Coarse facial features, increased head circumference, short neck, coarse hair, ear and respiratory infections, enlarged tongue, and hearing loss
3. Gastrointestinal signs2
Enlarged liver and spleen, hernias, diarrhea, difficulty in swallowing, heartburn, and intestinal inflammation
4. Musculoskeletal issues2,7
Abnormal development of all bones, joint pain and stiffness, short stature, joint contracture, scoliosis, kyphosis, hump, knock-knee, curved fingers, and restricted mobility
5. Ophthalmological complications2
Corneal clouding, heavy eyebrows, visual impairment, and photosensitivity
6. Dental issues2
Abnormal dentition with small and widely spaced teeth and enlarged gingiva
7. Cardiovascular signs2
Left ventricular hypertrophy, aortic insufficiency, mitral regurgitation, congestive cardiac failure, aortic stenosis, and thickened aortic and mitral valves
8. Pulmonary complications2,7
Decreased pulmonary function, obstructive airway disease, sleep apnea, and chronic bronchitis
It takes a team to manage MPS VII
Because MPS VII affects multiple organs and systems of the body, treatment requires a coordinated health care team. A patient will have several doctors from different specialty areas, including the following:
General Physician/Pediatrician
General health and medical care
Physiotherapist
Movement and physical function
Otolaryngologist
Ear, nose, and throat
Intensivist
Intensive care
Gastroenterologist
Stomach and intestines
Orthopedist
Skeleton and associated structures
Neurologist
Nervous system, including the brain, spinal cord, and nerves
Pulmonologist
Lungs
Dentist
Teeth, jaws, and mouth
Metabolic physician
Conditions that may have a chemical or biological basis
Rheumatologist
Inflammation or pain in muscles, joints, or tissue
Anesthesiologist
Administers medications during surgeries
Ophthalmologist
Eyes
Cardiologist
Heart
Infusion specialist
Administration of treatment
The geneticist will play a key role in MPS VII diagnosis and care. A geneticist takes the lead in
- Coordinating many aspects of your treatment plan
- Scheduling visits with specialists who monitor different symptoms
You may have many questions
To help plan for doctor visits, here are some sample questions for you to bring to your next appointment:
Diagnosis
- What tests are used to diagnose MPS VII?
- Do the tests hurt?
- Should other family members be tested?
Symptoms and lifestyle
- How can pain from MPS VII be managed?
- Is there a chance of heart problems?
- Do people with MPS VII lose their vision?
- Does MPS VII cause hearing trouble?
- Does it cause breathing problems?
- Are crutches or a wheelchair needed?
- Is a special diet required?
- How often should MPS VII patients have tests performed to monitor their health?
- What are safe ways to stay active?
- What do teachers or school nurses need to know about MPS VII?
Treatments and surgeries
- What treatment options are available?
- What are the risks and benefits of the different treatment options?
- Which specialists should be involved in treatment decisions, and how often?
- What types of surgeries are most common for people with MPS VII?
- What are the unique surgical risks that exist for people who have MPS VII?
- Have you ever operated on a person with MPS VII before?
- What tests are necessary before surgery?
- What are the risks of surgery?
- What’s important to know about being anesthetized (put under) before surgery?
- What will recovery be like?
MPS VII Resources
Patient advocacy organizations are located throughout the world to support and educate the MPS community
Along with tools and programs for patients, caregivers, and families, these organizations offer opportunities to meet others living with and impacted by MPS.
National MPS Society (United States)

- Memberships for individuals with MPS and their families
- Information and education
- Resources for advocacy and family support
- Pathways Program for newly diagnosed families
- Organized fundraisers and social events
- General clinical study information
MPS Europe is also available to help

- Support access to treatment and care for all MPS patients
- Educate and empower patients and patient representatives
- Provide materials for early diagnosis, clinical management, interventions, and treatment
- Organize and coordinate MPS Day activities and events for raising awareness
- Improve information flow about diagnostics, treatment, clinical studies, and standards of care among MPS societies
- Support national MPS societies in advocating access to medicines
- Represent MPS patients in the European Medicines Agency (EMA) and other European Union (EU) institutions and bodies
- Establish an MPS patient database on a European level
- Organize European and international conferences
- Support establishing MPS societies in developing countries
Other MPS organizations worldwide
Advocacy groups around the world champion awareness of all MPS diseases, including MPS VII. Click on the country’s name below to link to a local advocacy group.
References: 1.National MPS Society. A Guide to Understanding MPS. Durham, NC: National MPS Society. https://mpssociety.org/cms/wp-content/uploads/2017/04/MPS_VII_2008.pdf. Accessed August 14, 2018. 2. Montaño AM, Lock-Hock N, Steiner RD, et al. Clinical course of sly syndrome (mucopolysaccharidosis type VII). J Med Genet. 2016;53(6):403-418. 3. Fox JE, Volpe L, Bullaro J, Kakkis ED, Sly WS. First human treatment with investigational rhGUS enzyme replacement therapy in an advanced stage MPS VII patient. Mol Genet Metab. 2015;114(2):203-208. 4. Lehman TJA, Miller N, Norquist B, Underhill L, Keutzer J. Diagnosis of the mucopolysaccharidoses. Rheumatology (Oxford). 2011;50(suppl 5):v41-v48. 5. Mucopolysaccharidosis type 7. Orpha.net rare diseases search website. https://www.orpha.net/consor/cgi-bin/Disease_Search.php?lng=EN&data_id=40&Disease_Disease_Search_diseaseGroup=Mucopolysaccharidosis-type-7&Disease_Disease_Search_diseaseType=Pat&Disease(s)/group%20of%20diseases=Mucopolysaccharidosis-type-7&title=Mucopolysaccharidosis-type-7&search=Disease_Search_Simple. Accessed August 14, 2018. 6. Mucopolysaccharidosis type VII. National Institutes of Health Genetics Home Reference website. https://ghr.nlm.nih.gov/condition/mucopolysaccharidosis-type-vii. Accessed August 14, 2018. 7. Cimaz R, Coppa GV, Koné-Paut I, et al. Joint contractures in the absence of in indicate mucopolysaccharidosis. Pediatr Rheumatol Online J. 2009;7:18.








